Wisdom teeth extraction
In recent years there has been a lot of discussion about wisdom teeth or third molars – why should they be removed; when should they be removed; do they have to be removed? It seems everyone has an opinion, but there is one undeniable truth: When it comes to your wisdom teeth, the worst thing you can do is ignore them!
What are wisdom teeth?
Wisdom teeth are the last teeth to develop and appear in your mouth. They enter the mouth behind the upper and lower second or 12-year, molars between the ages of 17 and 25, a time of life that has been called the “Age of Wisdom.”
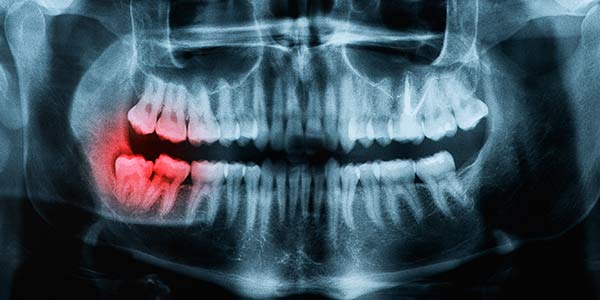
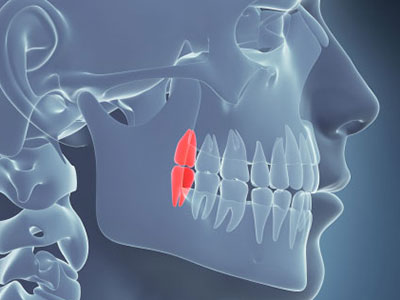
WHAT IS AN IMPACTED TOOTH?
Teeth are considered impacted if they are unable to erupt into the mouth.
WHY ARE IMPACTED WISDOM TEETH A CONCERN?
- Infection
- Damage to neighboring teeth and roots
- Tooth decay
- Periodontal disease
- Receding gums
- Loosened teeth
- Bone loss
- Tooth loss
More serious problems may occur if the sac surrounding the impacted tooth becomes filled with fluid and enlarges to form a cyst.
As the cyst grows it may hollow out the jaw and permanently damage neighboring teeth and the surrounding bone and nerves. Rarely, if a cyst is not treated, a tumor may develop from its walls and surgery may be needed to remove it.
It isn’t always wise to wait until your wisdom teeth start to bother you before having them removed
A young adult’s wisdom teeth have incomplete root systems, making the surgery to remove the teeth less complicated and the healing process is quicker.
As wisdom teeth grow, their roots lengthen and may become entangled with the sensory nerves that run throughthe lower jaw, or the sinus area. In these cases the wisdom teeth may be more difficult to remove and complications more likely to occur.
No one can predict when third molar complications will occur, but when they do, the circumstances can be much more painful and the teeth more difficult to treat if done later in life.
“Pain free” does not mean “disease free”
Because they are located in the back of the mouth, wisdom teeth are very difficult to keep clean. As a result, the bacteria that cause gum disease may exist in and around the teeth, leading to problems before pain or other symptoms let you know something is wrong.
Research also suggests this bacteria may travel through your bloodstream and contribute to other health problems including diabetes, heart disease and kidney disease.
Other studies suggest that gum disease in expectant mothers could be associated with a greater likelihood of preterm and low birthweight babies.
WHEN SHOULD I HAVE MY WISDOM TEETH REMOVED?
- A careful examination of your mouth
- A radiographic examination involving x-rays or a CT scan and
- A discussion with your dentist and oral and maxillofacial surgeon
Depending on the results of your dental examination your surgeon may:
- Extract the complete tooth
- Partially remove the tooth (coronectomy); or
- Observe the tooth over time for changes in condition.
In general, dental professionals agree that third molars should be removed whenever there is evidence of:
- Periodontal disease
- Cavities that cannot be restored
- Infections
- Cysts or tumors
- Damage to neighboring teeth
Third molars may not require surgery if they are:
- Completely erupted and functional
- Painless
- Free of cavities
- Disease free
- In a position that can be kept clean and healthy.
If after discussing your situation with your family dentist or surgeon you decide to keep your wisdom teeth for the time being, it’s important to agree on a long term plan for monitoring the health and condition of these teeth and their surrounding gum tissue.
Most oral surgeons recommend the following maintenance routine:
- Schedule a dental checkup at least annually
- X-rays or CT scans should be taken to see the wisdom teeth and surrounding bone
- A clinical examination should be performed annually to determine whether any disease is developing.
- Particular care must be taken to clean and floss the area as part of your daily oral healthcare regimen.
PREPARING FOR SURGERY
Most wisdom tooth extractions are routinely performed with little or no discomfort in the oral surgeon’s office.
- Plan to wear comfortable clothing with short sleeves or sleeves that can be easily rolled up.
- If your surgeon has recommended intravenous anesthesia, don’t eat or drink anything for six to eight hours before the procedure.
- Arrange for someone to see you home after the procedure.
Your surgeon will provide additional instructions before the day of surgery.,/p>
Immediately following surgery, you will rest in a recovery room until your surgeon determines you are able to return home. You will receive detailed instructions on what to do and what to expect after your surgery. If you have any questions, be sure to ask them before you leave the office.
THE SURGICAL PROCEDURE
The time required for the surgery and the type of surgical procedure used depends on several factors including position of the teeth, length and curvature of the roots, thickness of the bone surrounding the teeth and your physical condition and health.
If the teeth are fully erupted, it may be possible to simply remove each tooth intact from its socket in the bone, using instruments designed for this purpose.
If gum tissue is covering the tooth, an incision will be required to turn back the gum and expose the tooth.
If bone covers the tooth, the surgeon will remove sufficient bone to expose the tooth and allow its removal.
If an incision is needed to remove the tooth, your surgeon may place some sutures to help the wound heal.
Immediately following surgery you will rest for a time in the oral surgeon’s office before you leave for home with your escort.
AFTER YOUR SURGERY – WHAT TO EXPECT
Following are some additional suggestions you may find helpful:
- An ice pack may be used during the first 48-72 hours to help reduce temporary swelling and discoloration of the skin.
- Moist heat applied to the face may be helpful if your jaw is sore and you are unable to open your mouth as wide as usual.
- If bleeding is excessive after you return home of if you experience increased pain after the first 72 hours following surgery, contact your oral surgeon immediately for instructions.
- Gently open and close your mouth to help exercise the jaws and restore normal movement.
- Eat soft foods and drink fluids during the first two days after surgery, but avoid using straws as the suction could disturb clotting.
- Do not rinse your mouth vigorously until clotting is complete, although gentle rinsing with salt water may be recommended by your surgeon to aid in healing.
- Avoid eating hard or sticky foods that might damage your jawbone, particularly if bone was removed during surgery.
- Do not smoke as this may disturb blood clots and the healing process.
- Resume brushing your teeth the second day after surgery, but avoid disturbing blood clots with the toothbrush.
Medication prescribed your surgeon will help with any discomfort and you should generally be able to resume normal activities within a relatively short period of time.
KNOWN RISKS AND COMPLICATIONS
- Infection – any infection should be taken seriously and reported to your surgeon who will prescribe appropriate antibiotics to treat the problem. Signs of infection include fever, abnormal swelling and pain, salty or prolonged bad taste and pus formation.
- Injury – neighboring teeth, filling material or bridge work located near the wisdom teeth may be damaged during extraction.
- Dry socket – if a blood clot prematurely dissolves or does not form properly in the empty socket, for example due to smoking or food impaction, the socket remains “dry” for a period of time and heals more slowly than usual. A dry socket can be quite painful because it leaves the bone in the socket exposed to air, food and fluids. If you experience increases pain a few days after surgery, contact your surgeon. Steps can be taken to reduce discomfort while healing takes place.
- Numbness, or altered sensation – in some cases major sensory nerves are located near wisdom teeth, and it is possible that one or more of these nerves could be irritated during surgery. If this happens, you may experience altered or total loss of feeling in the lip, tongue, cheek, chin, gums or teeth, depending on the nerve that is involved. Although numbness beyond a relatively short period of time in any location is uncommon and usually temporary, it may be permanent in rare instances.
- Sinus complications – sometimes upper wisdom teeth are located near the large maxillary sinus and the roots may even penetrate into the sinus cavity. When removed, these wisdom teeth may leave an opening in the sinus that will usually heal without a problem. Rarely, drainage or sinus pain may occur following tooth removal. If these complications develop, contact your oral surgeon.
- Root fragments – occasionally tooth roots are extremely long or fragile and a piece may break off during surgery. Typically the fragment is removed, but if it is too close to a nerve or the sinus cavity, or if its removal would jeopardize adjacent teeth, the surgeon may decide to leave the fragment in place. This, rarely presents long-term problems, and the fragment can be monitored with x-rays.
- Jaw fracture – in very rare cases, the removal of wisdom teeth can weaken the jawbone, particularly if the jaw is thin and the teeth are severely impacted. If a fracture occurs, x-rays will reveal the location and your surgeon can treat the problem. Care should be taken to avoid eating hard, crunchy foods that place undue stress on the jaws until healing is completed.
- Jaw joint pain or abnormal jaw function – while this is a rare occurrence, further treatment may be necessary if you experience such pain. Prior to surgery, be sure to inform your surgeon about any pre-existing joint problems in your jaw.
